Cerebral thrombosis is a frequent disease in neurologic department and its natural recovery is difficult and there is no specific treatment due to the lack of regeneration capacity of neural tissue, which make it regarded as an intractable disease.
Experimental study to develop animal model similar to cerebral thrombosis and to treat it by using neural stem cells are being done widely over the world, thus many experiences and successes being achieved.
In the course of carrying out the policy of the Worker's Party of Korea for breaking through the cutting-edge of medical science, the Histology Department of Pyongyang Medical College of
Therefore, they have found the optimal condition for isolation, culture and differentiation of neural stem cell, and that there is moderate correlation between behavioral deficits in local cerebral ischemic reperfusion model and the volume of ischemic area.
This study have also shown that neural stem cells of neonatal rat are implanted into the focal cerebral tissue of model animal.
These findings might provide basic materials for cerebral ischemic model experiments in which neural stem cells isolated from brain tissue of neonatal rat are used to treat ischemic brain injury of rat and clinical practice.
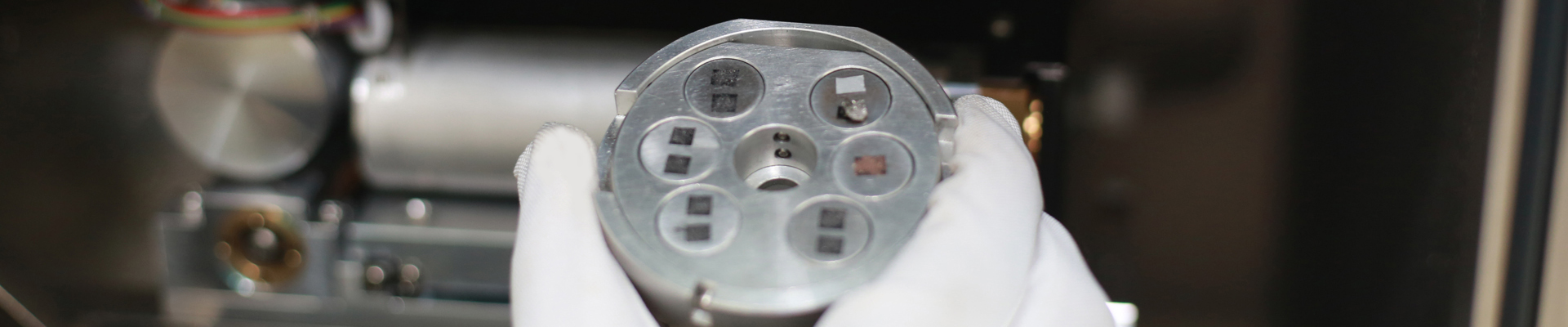
Isolation and culture of neural stem cells underwent enzymatically digestion of brain tissue of neonatal rat, primary culture and subculture of isolated cells.
They confirmed the culture of isolated neural stem cells by measuring the number of neurospheres and the amplification index, evaluating the survival rate of the cells and identifying the expression of Nestin in the cultured cells.
They occluded the middle cerebral artery to make the local cerebral ischemic reperfusion model.
The examination of animal model was performed by evaluating neurological impairment and measuring the ischemic area
After the injection of neural stem cells into the caudal vein of model rat, they evaluated the implanting capacity of neural stem cells in damaged brain tissue.
The brain tissue of neonatal rat was digested by 0.1% trypsin/0.1M EDTA for 10 min and the number of neurospheres and amplification index was increased as the age of animal was young.
During primary culture, the isolated cells had been incubated in 5×105/mL implantiation density and for 10d in the medium which contained 20ng/mL bFGF and EGF, 2% N2 and B27 and was exchanged once per 5 or 6days.
For their subsequent culture, neurospheres digested by 0.1% trypsin for 4min had been incubated 105/mL for 8d.
Their proliferating capacity was maintained even in the fourth generation.
The cultured neural stem cells were Nestin-positive.
As a result, they have found that there were moderate correlation between behavioral deficits and the volume of ischemic area in the local cerebral ischemic reperfusion model rat and neonatal rat,s brain-derived neural stem cells were implanted into the focal cerebral tissue of model animal.
In the future, they want to deep the research and perform actively also a cooperative research in order to increase survival rate of transplanted neonatal rat,s cerebral neural stem cells, differentiate to nerve cell and give an answer regenerative effect of brain tissue in focal region.